There are currently two main ways to receive a definitive Barth syndrome diagnosis: genetic testing forTAFAZZIN variants and/or analysis of the monolysocardiolipin (MLCL) to cardiolipin (CL) ratio (MLCL/CL) via mass spectrometry.
FOR PROVIDERS

GENETIC TESTING
Pathogenic mutations in TAFAZZIN cause Barth syndrome. Mutations in TAFAZZIN can be inherited or de novo; lack of family history does not rule out diagnosis of Barth syndrome. Several options exist for identification of TAFAZZIN mutations: genomic panels, whole exome sequencing and whole genome sequencing. While whole genome sequencing offers the most comprehensive survey of coding and non-coding sequences, the turnaround time and cost may impact election of this method over more targeted approaches like whole exome sequencing or gene panels based on disease areas (e.g. cardiomyopathy, arrhythmia and metabolic panels). A list of available commercial tests can be found via the Genetic Testing Registry (GTR®), which includes the test's purpose, methodology, validity, evidence of the test's usefulness, and laboratory contacts and credentials.
Upon identification of a TAFAZZIN mutation, resources such as the Human TAFAZZIN Gene Variants Database curated by BSF or websites such as ClinVar or gnomAD can be consulted to determine pathogenicity. If a variant is of unknown significance (i.e. VUS) or whole exome/panel sequencing is not informative but there is strong clinical suspicion for Barth syndrome, a blood sample should be evaluated for the MLCL/CL ratio (see below) for confirmation of diagnosis.
MLCL/CL RATIO ASSAY
Cardiolipin testing provides a biochemical approach to testing. Measurements of monolysocardiolipin (MLCL) and cardiolipin (CL) have been shown to have high specificity and sensitivity for Barth syndrome using only a small volume of blood (5 mL), patient-derived fibroblast cell lysates, or dried blood spots. Testing can be requested through the Laboratory of Genetic Metabolic Diseases (LGMD) University Medical Center, Amsterdam and results are typically available within a few weeks. To our knowledge, the LGMD at Amsterdam University Medical Center is the only lab currently approved to offer CLIA-equivalent, clinical testing for MLCL/CL. To request testing, complete this form and follow instructions within the form for sample submission. Gene testing should still be performed as further confirmation in someone with a positive cardiolipin test.
FOR AFFECTED FAMILIES

GENETIC TESTING
Variants, also called mutations, are defined as changes to the DNA sequence. Sometimes changes to DNA are passed down from parents to children (i.e. inherited) while other times, variations in the DNA sequence can appear spontaneously in a developing embryo (i.e. de novo). Many changes are benign, meaning that they don’t have an impact on the gene’s function. Other variants are considered pathogenic, where the change negatively impacts the way a gene does its job. Scientists can “read” these changes by looking at all of the individual DNA building blocks and comparing them to a known, non-Barth sample. Changes in the gene TAFAZZIN can cause Barth syndrome. A list of genetic tests that your doctor or genetic counselor can order can be found here.
MLCL/CL RATIO ASSAY
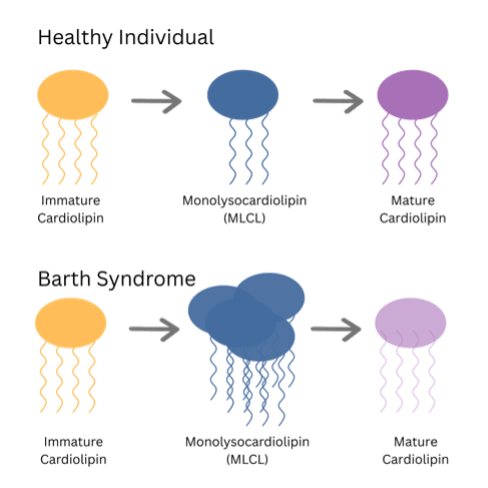
Cardiolipin is an important fat (also known as a lipid) that helps mitochondria form a barrier called a membrane. Mitochondria are special components of cells that make energy. Membranes are physical structures that help mitochondria keep their shape and function properly. A lab test has been developed that can measure different types of cardiolipin, which can aid in diagnosing Barth syndrome. This test is currently only available through a lab in the Netherlands; your doctor can order this test using this link.
More in-depth description of MLCL/CL Testing:
Cardiolipin (represented in the above drawing) has four “legs” (i.e. fatty acid side chains). Cardiolipin undergoes a special process called remodeling where one “leg” is removed to produce an intermediate form called monolysocardiolipin, or MLCL for short. In the final step to make mature cardiolipin, the form that mitochondria use to make their membranes, a new “leg” is added back via TAFAZZIN. In Barth syndrome, changes to the TAFAZZIN sequence (i.e. variants) prevent it from adding back the 4th “leg”, leading to a pile-up of MLCL. This build-up of MLCL is very specific to Barth syndrome and can be measured by a sophisticated lab test called mass spectrometry (learn more here) to determine if someone with the symptoms of Barth syndrome actually has the condition. In combination with genetic sequencing, the MLCL/CL ratio helps doctors understand whether a person has Barth syndrome.



